Program Description
Of the 5 to 12% U.S. adults living with serious illness, many are at risk for preventable suffering. As health care organizations drive toward value, the need to provide higher quality, cost-efficient care for this high-risk, high-need population is vital. The Center to Advance Palliative Care (CAPC) worked closely with commercial and Medicare Advantage health plans as well as Accountable Care Organizations (ACOs) across the country to define a population health approach to care for people with serious illness that ensures better experiences for both patients and caregivers with significantly lower cost. Evidence also exists that this approach bolsters clinician experience.
The “Serious Illness Strategies Driving Value in High-Need Populations” monograph outlines three key strategies: proactively identifying seriously ill individuals, engaging with patients and caregivers to assess their distress, and providing home-based care to support the highest-need patients. Payers using these strategies report improved patient outcomes and reduced total cost of care.
“Health care leaders have a tremendous opportunity at hand—to help families through a difficult experience while simultaneously optimizing value in health care delivery. With a growing consensus on the highest impact strategies, new standards of care are being set for care of our sickest and most complex patients.”
Diane E. Meier, MD Founder, Director Emerita, and Strategic Medical Advisor Center to Advance Palliative Care
Impact
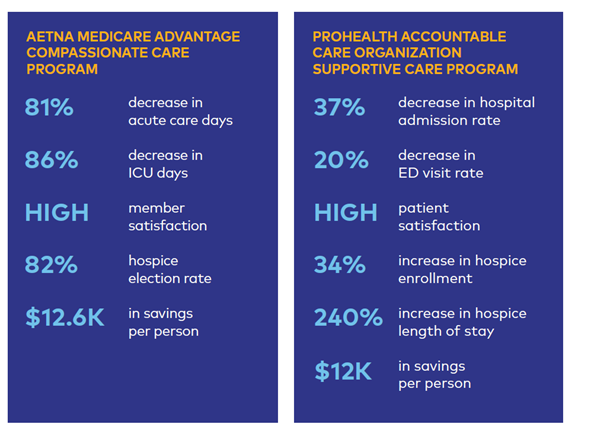
Early identification, comprehensive assessment, and targeted use of home-based care results in:
- Improved Patient and Family Experiences: Meaningful conversations, shared decision-making, and action plans to address pain and other symptoms dramatically improve satisfaction scores.
- Reductions in Emergency Department and Hospital Utilization: By identifying families at-risk of crisis and working to control symptoms and stress, these strategies have reduced unnecessary ED visits and acute care admissions by an average of 15%.
- Cost Savings: The strategies outlined result in significant cost savings, with examples like Aetna’s Compassionate Care program saving $12K per patient
To read the full publication, visit our resources page at: TBD
To access other free resources for health plans, ACOs, and purchasers visit: www.capc.org/toolkits/resources-for-health-plans